Ventilation and Gas Exchange
How we breathe and exchange oxygen and carbon dioxide
Every Breath You Take
The mechanics of breathing and gas exchange
Ventilation (breathing) is the movement of air into and out of the lungs. It's controlled by the diaphragm and intercostal muscles (muscles between the ribs), which change the volume of the thoracic cavity to create pressure differences.
Inspiration (Breathing In)
- Diaphragm contracts and flattens downward
- Intercostal muscles contract, pulling ribs up and out
- Volume increases in the thoracic cavity
- Pressure decreases below atmospheric pressure
- Air rushes in to equalize pressure
Expiration (Breathing Out)
- Diaphragm relaxes and curves upward
- Intercostal muscles relax, ribs move down and in
- Volume decreases in the thoracic cavity
- Pressure increases above atmospheric pressure
- Air is pushed out to equalize pressure
Key Point:
Breathing is based on pressure changes. Air always moves from high to low pressure.
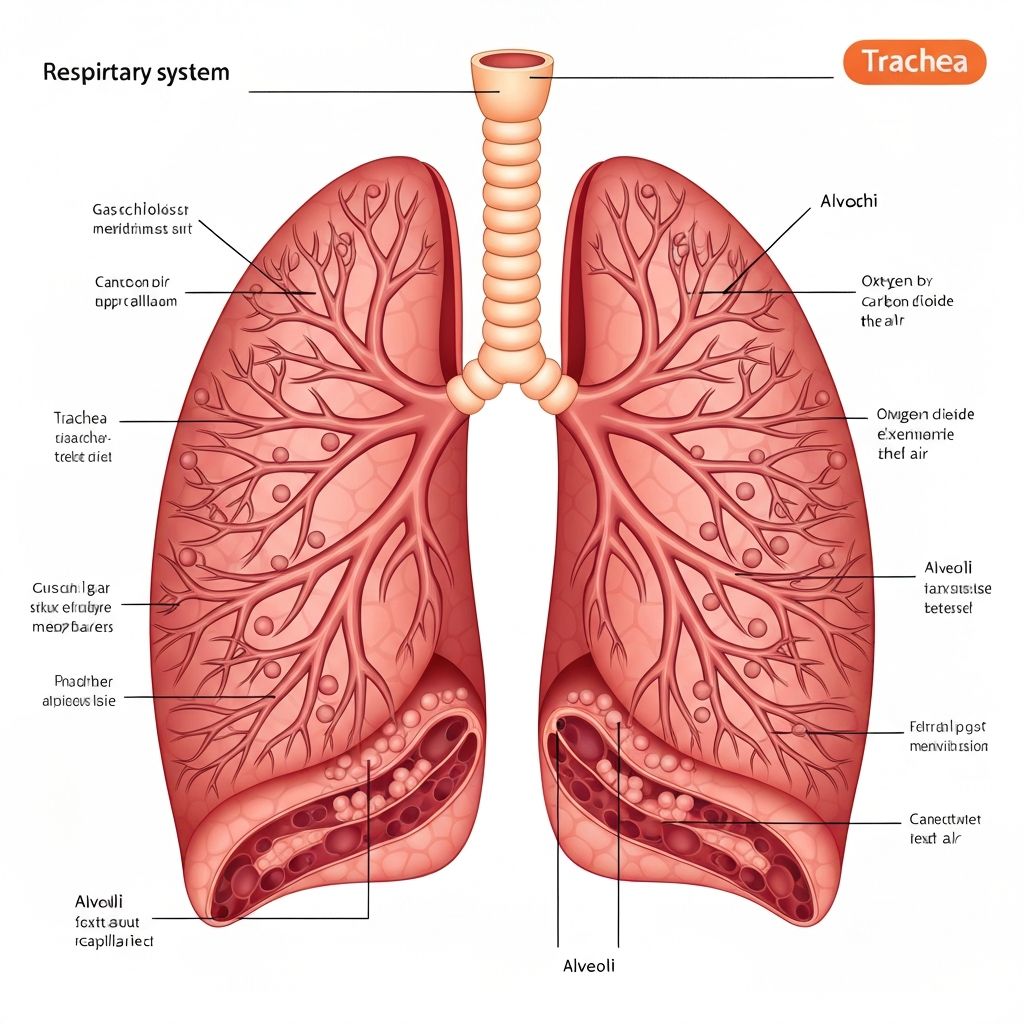
Gas exchange occurs in two main locations: in the lungs (between air and blood) and in the tissues (between blood and cells). This exchange happens by diffusion, moving from areas of high to low concentration.
At the Lungs (Alveoli)
- Oxygen diffuses from air (high concentration) into blood (low concentration)
- Carbon dioxide diffuses from blood (high concentration) into air (low concentration)
- Gases cross the alveolar and capillary walls
At the Tissues (Body Cells)
- Oxygen diffuses from blood (high concentration) into cells (low concentration)
- Carbon dioxide diffuses from cells (high concentration) into blood (low concentration)
- Gases cross the capillary walls and cell membranes
The alveoli (tiny air sacs in the lungs) have several adaptations that make gas exchange very efficient:
1. Large Surface Area
Millions of alveoli provide a huge surface area (about 70 m² - the size of a tennis court!) for gas exchange.
2. Thin Walls
Alveolar walls are only one cell thick, and so are capillary walls. This means gases only have to diffuse a very short distance.
3. Rich Blood Supply
Dense network of capillaries around each alveolus maintains steep concentration gradients by constantly bringing deoxygenated blood and removing oxygenated blood.
4. Moist Lining
A thin layer of moisture allows gases to dissolve before diffusing across membranes.
Oxygen Transport
- Most oxygen (about 97%) binds to hemoglobin in red blood cells, forming oxyhemoglobin
- Small amount (about 3%) dissolves directly in blood plasma
- Hemoglobin can carry 4 oxygen molecules per molecule
- Oxygen binds in the lungs (high O₂ concentration) and is released at tissues (low O₂ concentration)
Carbon Dioxide Transport
- About 70% is converted to bicarbonate ions (HCO₃⁻) in red blood cells and transported in plasma
- About 23% binds to hemoglobin, forming carbaminohemoglobin
- About 7% dissolves directly in plasma
- CO₂ is picked up at tissues and released at the lungs
Asthma
Airways become inflamed and narrow, making it difficult to breathe. Triggered by allergens, exercise, or cold air. Treated with inhalers that relax airway muscles.
Emphysema
Alveoli walls break down, reducing surface area for gas exchange. Often caused by smoking. Results in breathlessness and reduced oxygen in blood.
Cystic Fibrosis
Genetic condition causing thick, sticky mucus to build up in lungs. Makes breathing difficult and increases infection risk. Requires daily physiotherapy and medication.
Inspiration (Breathing In)
1. Diaphragm contracts (moves down)
2. Intercostal muscles contract (ribs up & out)
3. Volume increases → Pressure decreases
4. Air flows in from outside
Expiration (Breathing Out)
1. Diaphragm relaxes (moves up)
2. Intercostal muscles relax (ribs down & in)
3. Volume decreases → Pressure increases
4. Air is pushed out
Alveolus (Air Sac) & Capillary
Air in Alveolus
High O₂ concentration
Blood in Capillary
Low O₂ concentration
→ O₂ diffuses from AIR into BLOOD (high to low concentration)
Blood in Capillary
High CO₂ concentration
Air in Alveolus
Low CO₂ concentration
→ CO₂ diffuses from BLOOD into AIR (high to low concentration)
Term
Ventilation
Click to reveal definition
Question:
Explain why blood reaching the muscles during exercise has less oxygen than blood at rest, and what happens to the carbon dioxide levels.
Answer:
Why oxygen levels are lower:
- During exercise, muscle cells undergo increased respiration to release more energy for contraction
- This means they use more oxygen from the blood
- The concentration of oxygen in muscle cells becomes very low
- A steeper concentration gradient forms between the blood and muscle cells
- More oxygen diffuses out of the blood and into the muscle cells
- Hemoglobin releases more of its bound oxygen, so blood leaving the muscles has less oxygen than normal
What happens to carbon dioxide:
- Increased respiration produces more CO₂ as a waste product
- CO₂ concentration in muscle cells increases
- CO₂ diffuses from cells into blood down the concentration gradient
- Blood leaving the muscles has higher CO₂ levels than at rest
- This CO₂-rich blood travels to the lungs where CO₂ is exhaled
- Breathing rate increases to remove the extra CO₂ and bring in more oxygen
Summary:
Exercise increases cellular respiration in muscles, causing more oxygen to be used and more CO₂ to be produced. This creates steeper concentration gradients for both gases, resulting in more efficient gas exchange at the tissues.
What happens to the diaphragm during inspiration?